Gastroshiza, sometimes spelled gastroshisis or gastroschisis, is a serious but treatable congenital condition in which a baby is born with the intestines outside the abdominal wall. We’ll break down what gastroshiza means, how it’s detected early, and what modern management looks like to improve survival outcomes. Early diagnosis and coordinated neonatal care significantly increase the chances of full recovery, making awareness crucial for expecting parents and healthcare providers.
What Is Gastroshiza? (Definition & Overview)
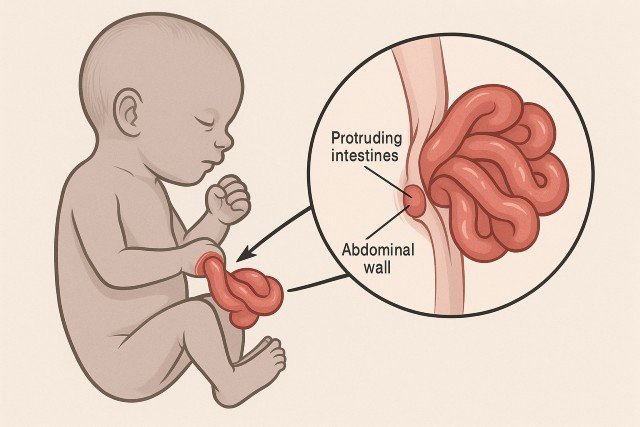
gastroshiza is a birth defect where the abdominal wall fails to close during fetal development, allowing the bowel — and sometimes other organs such as the stomach or liver — to protrude outside the body through a small opening near the belly button.
Key Characteristics of Gastroshiza
- A defect typically to the right of the umbilical cord
- Intestines are not covered by a protective sac (unlike omphalocele)
- Requires immediate medical attention after birth
- Often detected during routine prenatal ultrasound
Gastroshiza vs. Omphalocele: A Quick Comparison
| Feature | Gastroshiza | Omphalocele |
|---|---|---|
| Organ covering | No protective sac | Covered by sac |
| Opening location | Right of umbilical cord | Midline defect |
| Associated anomalies | Less common | More common |
| Risk factors | Younger mothers, certain environmental exposures | Chromosomal abnormalities |
Primary Causes and Risk Factors
While the exact cause of gastroshiza remains unclear, researchers believe a mix of environmental and genetic factors contribute to the defect.
Commonly Associated Risk Factors
- Young maternal age (under 20 years)
- Smoking or alcohol consumption during pregnancy
- Recreational drug exposure
- Nutritional deficiencies
- Environmental toxins such as pesticides
- Low socioeconomic status
- Maternal infection or inflammation
What the Research Says
According to the U.S. Centers for Disease Control and Prevention (CDC), gastroschisis occurs in about 1 in every 1,900 births, with rates increasing in younger mothers.
How Gastroshiza Is Diagnosed: Early Detection Matters
1. Prenatal Ultrasound (Primary Diagnostic Tool)
Gastroshiza can typically be seen on an ultrasound between 18 and 20 weeks of pregnancy. The exposed intestines appear as floating loops outside the fetal abdomen.
2. Maternal Serum Alpha-Fetoprotein (MSAFP)
Elevated AFP levels during pregnancy may indicate abdominal wall defects.
3. Fetal MRI (For Complex Cases)
MRI gives a more detailed image of the bowel condition and helps with surgical planning.
Types of Gastroshiza
Simple Gastroshiza
- Only intestines protrude
- No major complications
- Faster recovery after birth
Complex Gastroshiza
- Bowel damage due to twisting or inflammation
- Possible involvement of stomach or liver
- Requires advanced surgical and neonatal care
Management Options for Gastroshiza
1. Prenatal Management
Once diagnosed, the pregnancy becomes high-risk and requires:
- Frequent ultrasound monitoring
- Assessment of fetal growth
- Planning for delivery at a facility with NICU and pediatric surgery availability
- Avoidance of premature delivery unless medically necessary
2. Delivery Planning
Vaginal delivery is often safe; however, a cesarean section may be recommended in complex cases.
Postnatal Treatment: What Happens After Birth
Treatment focuses on protecting the exposed organs, preventing infection, and repairing the abdominal wall.
Step-by-Step Management Process
1. Immediate Stabilization
- Baby is placed in a sterile bag to protect bowel tissue
- Nasogastric tube insertion
- Intravenous (IV) fluids and antibiotics
- Body temperature stabilization
2. Surgical Repair Options
Primary Closure
- Performed when organs can be placed back inside safely
- One-time surgery
Staged Closure (Silo Method)
- Used when bowel swelling prevents immediate closure
- A “silo bag” gradually returns organs into the abdomen over several days
3. Recovery and Long-Term Care
- Nutrition via IV (Total Parenteral Nutrition) until bowel function improves
- Gradual introduction of breast milk or formula
- Monitoring for complications such as infection, narrowed bowel, or feeding intolerance
Prognosis and Long-Term Outcomes
With proper treatment, survival rates exceed 90% for infants with simple gastroshiza. Outcomes depend on the extent of bowel damage and the presence of complications.
Potential Long-Term Considerations
- Feeding difficulties
- Slow weight gain
- Short bowel syndrome (rare)
- Gastrointestinal motility issues
- Need for long-term nutrition support (in complex cases)
Prevention Tips: Can Gastroshiza Be Avoided?
While not always preventable, certain practices lower the risk:
- Avoid smoking, alcohol, and drugs during pregnancy
- Take prenatal vitamins with folic acid
- Maintain proper nutrition
- Limit exposure to harmful chemicals
- Attend regular prenatal checkups
Frequently Asked Questions (FAQ) About Gastroshiza
1. Is gastroshiza life-threatening?
Not necessarily. With early diagnosis and proper neonatal care, most babies recover fully.
2. Can gastroshiza be detected in the first trimester?
Yes, in some cases. High-resolution ultrasound can detect abnormalities as early as 12–13 weeks.
3. Do babies with gastroshiza have long-term disabilities?
Most do not. Simple gastroshiza typically results in normal long-term growth and development.
4. Is surgery always required?
Yes. Surgical repair is essential to return organs to the abdomen and close the defect.
5. Can a mother deliver naturally?
Often yes, but a C-section may be recommended for complex cases.
Conclusion
Understanding gastroshiza — from early diagnosis to postnatal management — empowers families and healthcare providers to prepare for the best care possible. While the condition can be alarming, modern medical advancements have dramatically improved outcomes. With timely detection, skilled surgical intervention, and comprehensive neonatal support, most infants with gastroshiza go on to live healthy, fulfilling lives.
If you are seeking more detailed insights or personalized guidance, ensure your information comes from reliable healthcare providers and reputable sources like the CDC or American Academy of Pediatrics.